On this page:
- What is tinnitus?
- What causes tinnitus?
- Why do I have this noise in my ears?
- What should I do if I have tinnitus?
- What if the sounds in my ear do not go away?
- Are there treatments that can help me?
- Can I do anything to prevent tinnitus or keep it from getting worse?
- What are researchers doing to better understand tinnitus?
- Where can I find additional information about tinnitus?
What is tinnitus?
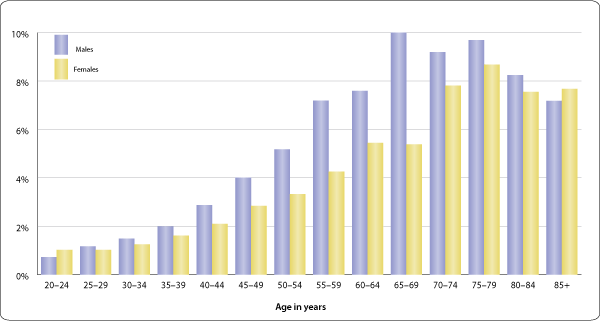
Tinnitus is commonly described as a ringing in the ears, but it also can sound like roaring, clicking, hissing, or buzzing. It may be soft or loud, high pitched or low pitched. You might hear it in either one or both ears. Roughly 10 percent of the adult population of the United States has experienced tinnitus lasting at least five minutes in the past year. This amounts to nearly 25 million Americans.
What causes tinnitus?
Tinnitus (pronounced tin-NY-tus or TIN-u-tus) is not a disease. It is a symptom that something is wrong in the auditory system, which includes the ear, the auditory nerve that connects the inner ear to the brain, and the parts of the brain that process sound. Something as simple as a piece of earwax blocking the ear canal can cause tinnitus. But it can also be the result of a number of health conditions, such as:
- Noise-induced hearing loss
- Ear and sinus infections
- Diseases of the heart or blood vessels
- Ménière’s disease
- Brain tumors
- Hormonal changes in women
- Thyroid abnormalities
Tinnitus is sometimes the first sign of hearing loss in older people. It also can be a side effect of medications. More than 200 drugs are known to cause tinnitus when you start or stop taking them.
People who work in noisy environments—such as factory or construction workers, road crews, or even musicians—can develop tinnitus over time when ongoing exposure to noise damages tiny sensory hair cells in the inner ear that help transmit sound to the brain. This is called noise-induced hearing loss.
Service members exposed to bomb blasts can develop tinnitus if the shock wave of the explosion squeezes the skull and damages brain tissue in areas that help process sound. In fact, tinnitus is one of the most common service-related disabilities among veterans returning from Iraq and Afghanistan.
Pulsatile tinnitus is a rare type of tinnitus that sounds like a rhythmic pulsing in the ear, usually in time with your heartbeat. A doctor may be able to hear it by pressing a stethoscope against your neck or by placing a tiny microphone inside the ear canal. This kind of tinnitus is most often caused by problems with blood flow in the head or neck. Pulsatile tinnitus also may be caused by brain tumors or abnormalities in brain structure.
Even with all of these associated conditions and causes, some people develop tinnitus for no obvious reason. Most of the time, tinnitus isn’t a sign of a serious health problem, although if it’s loud or doesn’t go away, it can cause fatigue, depression, anxiety, and problems with memory and concentration. For some, tinnitus can be a source of real mental and emotional anguish.
Why do I have this noise in my ears?
Although we hear tinnitus in our ears, its source is really in the networks of brain cells (what scientists call neural circuits) that make sense of the sounds our ears hear. A way to think about tinnitus is that it often begins in the ear, but it continues in the brain.
Scientists still haven’t agreed upon what happens in the brain to create the illusion of sound when there is none. Some think that tinnitus is similar to chronic pain syndrome, in which the pain persists even after a wound or broken bone has healed.
Tinnitus could be the result of the brain’s neural circuits trying to adapt to the loss of sensory hair cells by turning up the sensitivity to sound. This would explain why some people with tinnitus are oversensitive to loud noise.
Tinnitus also could be the result of neural circuits thrown out of balance when damage in the inner ear changes signaling activity in the auditory cortex, the part of the brain that processes sound. Or it could be the result of abnormal interactions between neural circuits. The neural circuits involved in hearing aren’t solely dedicated to processing sound. They also communicate with other parts of the brain, such as the limbic region, which regulates mood and emotion.
What should I do if I have tinnitus?
The first thing is to see your primary care doctor, who will check if anything, such as ear wax, is blocking the ear canal. Your doctor will ask you about your current health, medical conditions, and medications to find out if an underlying condition is causing your tinnitus.
If your doctor cannot find any medical condition responsible for your tinnitus, you may be referred to an otolaryngologist (commonly called an ear, nose, and throat doctor, or an ENT). The ENT will physically examine your head, neck, and ears and test your hearing to determine whether you have any hearing loss along with the tinnitus. You might also be referred to an audiologist who can also measure your hearing and evaluate your tinnitus.
What if the sounds in my ear do not go away?
Some people find their tinnitus doesn’t go away or it gets worse. In some cases it may become so severe that you find it difficult to hear, concentrate, or even sleep. Your doctor will work with you to help find ways to reduce the severity of the noise and its impact on your life.
Are there treatments that can help me?
Tinnitus does not have a cure yet, but treatments that help many people cope better with the condition are available. Most doctors will offer a combination of the treatments below, depending on the severity of your tinnitus and the areas of your life it affects the most.
- Hearing aids often are helpful for people who have hearing loss along with tinnitus. Using a hearing aid adjusted to carefully control outside sound levels may make it easier for you to hear. The better you hear, the less you may notice your tinnitus. Read the NIDCD fact sheet Hearing Aids for more information.
- Counseling helps you learn how to live with your tinnitus. Most counseling programs have an educational component to help you understand what goes on in the brain to cause tinnitus. Some counseling programs also will help you change the way you think about and react to your tinnitus. You might learn some things to do on your own to make the noise less noticeable, to help you relax during the day, or to fall asleep at night.
- Wearable sound generators are small electronic devices that fit in the ear and use a soft, pleasant sound to help mask the tinnitus. Some people want the masking sound to totally cover up their tinnitus, but most prefer a masking level that is just a bit louder than their tinnitus. The masking sound can be a soft “shhhhhhhhhhh,” random tones, or music.
- Tabletop sound generators are used as an aid for relaxation or sleep. Placed near your bed, you can program a generator to play pleasant sounds such as waves, waterfalls, rain, or the sounds of a summer night. If your tinnitus is mild, this might be all you need to help you fall asleep.
- Acoustic neural stimulation is a relatively new technique for people whose tinnitus is very loud or won’t go away. It uses a palm-sized device and headphones to deliver a broadband acoustic signal embedded in music. The treatment helps stimulate change in the neural circuits in the brain, which eventually desensitizes you to the tinnitus. The device has been shown to be effective in reducing or eliminating tinnitus in a significant number of study volunteers.
- Cochlear implants are sometimes used in people who have tinnitus along with severe hearing loss. A cochlear implant bypasses the damaged portion of the inner ear and sends electrical signals that directly stimulate the auditory nerve. The device brings in outside sounds that help mask tinnitus and stimulate change in the neural circuits. Read the NIDCD fact sheet Cochlear Implants for more information.
- Antidepressants and antianxiety drugs might be prescribed by your doctor to improve your mood and help you sleep.
- Other medications may be available at drugstores and on the Internet as an alternative remedy for tinnitus, but none of these preparations has been proved effective in clinical trials.
Can I do anything to prevent tinnitus or keep it from getting worse?
Noise-induced hearing loss, the result of damage to the sensory hair cells of the inner ear, is one of the most common causes of tinnitus. Anything you can do to limit your exposure to loud noise—by moving away from the sound, turning down the volume, or wearing earplugs or earmuffs—will help prevent tinnitus or keep it from getting worse.
What are researchers doing to better understand tinnitus?
Along the path a hearing signal travels to get from the inner ear to the brain, there are many places where things can go wrong to cause tinnitus. If scientists can understand what goes on in the brain to start tinnitus and cause it to persist, they can look for those places in the system where a therapeutic intervention could stop tinnitus in its tracks.
In 2009, the National Institute on Deafness and Other Communication Disorders (NIDCD) sponsored a workshop that brought together tinnitus researchers to talk about the condition and develop fresh ideas for potential cures. During the course of the workshop, participants discussed a number of promising research directions, including:
- Electrical or magnetic stimulation of brain areas involved in hearing. Implantable devices already exist to reduce the trembling of Parkinson’s disease and the anxieties of obsessive-compulsive disorder. Similar devices could be developed to normalize the neural circuits involved in tinnitus.
- Repetitive transcranial magnetic stimulation (rTMS). This technique, which uses a small device placed on the scalp to generate short magnetic pulses, is already being used to normalize electrical activity in the brains of people with epilepsy. Preliminary trials of rTMS in humans, funded by the NIDCD, are helping researchers pinpoint the best places in the brain to stimulate in order to suppress tinnitus. Researchers are also looking for ways to identify which people are most likely to respond well to stimulation devices.
- Hyperactivity and deep brain stimulation. Researchers have observed hyperactivity in neural networks after exposing the ear to intense noise. Understanding specifically where in the brain this hyperactivity begins and how it spreads to other areas could lead to treatments that use deep brain stimulation to calm the neural networks and reduce tinnitus.
- Resetting the tonotopic map. Researchers are exploring how to take advantage of the tonotopic map, which organizes neurons in the auditory cortex according to the frequency of the sound to which they respond. Previous research has shown a change in the organization of the tonotopic map after exposing the ear to intense noise. By understanding how these changes happen, researchers could develop techniques to bring the map back to normal and relieve tinnitus.
Where can I find additional information about tinnitus?
The NIDCD maintains a directory of organizations that provide information on the normal and disordered processes of hearing, balance, taste, smell, voice, speech, and language.
Use the following keywords to help you find organizations that can answer questions and provide information on tinnitus: