Digestive Problems in Sjogren's
Esophageal dysmotility has been reported in 36% to 90% of patients. Esophageal motility disorders involve dysfunction of the esophagus that causes symptoms such as difficulty swallowing, and heartburn.
Routine laboratory testing frequently reveals mild pancreatitis or hepatitis.
Hepatic involvement is seen in approximately 7% of patients with primary SS by the presence of antimitochondrial antibodies and, less frequently, by abnormal liver enzyme levels.
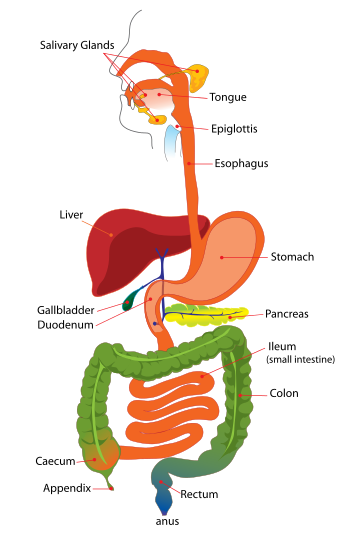
Inflammation in the esophagus, stomach, pancreas, and liver can cause problems like painful swallowing, heartburn, abdominal pain and swelling, loss of appetite, diarrhea, and weight loss. It can also cause hepatitis (inflammation of the liver) and cirrhosis (hardening of the liver).
Sjögren's is closely linked to a liver disease called primary biliary cirrhosis (PBC), which causes itching, fatigue, and, eventually, cirrhosis. Many patients with PBC have Sjögren's. NIAMS/National Institutes of Health
Sjogren’s can lead to gastroparesis or irritable bowel syndrome which both cause abdominal pain. Gastroparesis is a condition in which the stomach cannot empty normally. Signs include nausea, vomiting and weight loss.
The symptoms of irritable bowel syndrome include bloating, constipation and diarrhea. Medicine Net
Dysbiosis and Sjogren's syndrome
Dysbiosis is defined as negative alterations in the gut microbiome. Find out mare about it and what can help it here.
Visit the sjogren's blog where you can join in the conversation
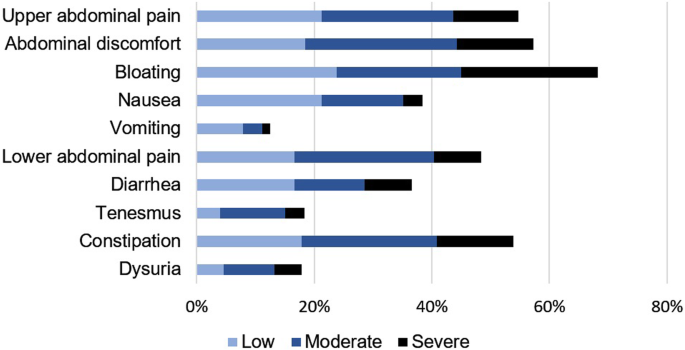
Abdominal symptoms during Sjogren’s syndrome: a pilot study published in January 2021.
Abdominal symptoms
Ninety-five percent of the patients, in this study, suffered from abdominal symptoms. The abdominal complaints are shown according to severity in Fig. 1. More than half of the patients had upper abdominal pain, abdominal discomfort, bloating and/or constipation.
Saliva normally plays a major role in neutralizing gastric acidity. Thus, symptoms of “heartburn” or “hiatal hernia” are common in Sjögren’s syndrome.
- Gastric hyperacidity can be partly overcome by the use of antacids (such as Mylanta II or Maalox II) after meals and at bedtime.
- Elevation of the head of the bed on 2- inch wood blocks provides a way to reduce the gastric acid from washing back into the esophagus at night.
- In some patients with severe problems of “heartburn,” the medicine sucralfate (Carafate slurry) has been helpful. This medicine was designed to “coat” the esophagus and stomach of patients with ulcer disease. However, sucralfate coating of the stomach might interfere with the absorption of certain other medications so be certain to check this possible drug interaction with your physician and pharmacist.
- For more severe heartburn, two types of medications decrease the response of the gastric mucosa to the acid or to reduce the gastric production of acid. The first type is called “H2 blockers” and includes Tagamet, Pepsid, and Zantac; each of these have recently become available over the counter. A second type of medication that reduces acid production still requires a prescription. Members of this family include Prilosec (Omerasol in Mexico), which will soon go over the counter, as well as Nexium, Aciphex, Prevacid, and Protonix. There has been debate about whether a combination of these medications is more useful than either class alone. If a combination is taken, then the acid suppressor (i.e.Prilosec like) might be taken in the morning, while the H2 blocker (i.e. tagamet) might be taken before bed.
- Finally, some patients who have decreased motility of the esophagus benefited from a medicine called cisapride (Propulsid). However, this medication was removed from the market in the US due to a relatively rare side effect after many years of use with a good overall safety record. Reglan, Other medications with similar beneficial effects are in the late stages of clinical development and should reach the market in near future.
- Since saliva normally helps during swallowing pills, it is important to recognize that pills can become stuck to “dry” walls of the esophagus and cause painful erosions. For example, iron supplement pills are large in size and uncoated tablets may get stuck in the esophagus, leading to pain and a choking sensation. Also, certain time-release preparations tend to adhere to the esophagus in the absence of sufficient saliva. To minimize these problems, coated tablets are preferred (when available) and medication should be taken with lots of water while sitting in the upright position (rather than lying down just after taking the pills).
Let’s talk about acidic foods. Do they all behave similarly once ingested?
Not all acidic foods behave the same when ingested. The pH value of food tells you if something is an acid, a base, or neutral.
- A pH of 0 indicates a high level of acidity.
- A pH of 7 is neutral.
- A pH of 14 is the most basic, or alkaline.
Interestingly, some foods [like many fruits and veggies] have a naturally low pH but are actually alkalizing when digested. Neither the pH of your blood nor cells can be altered by what you eat as the pH of the body is controlled mainly by the kidneys.
The more acidic the food, theoretically, the more likely it is to cause gastrointestinal distress by triggering GERD (Gastroesophageal Reflux Disease). Having said that, every person is different, and although some acidic foods may be intolerable to one group of patients, they may be perfectly tolerable to another.
Selective elimination of dietary triggers (fatty foods, caffeine, chocolate, spicy foods, carbonated beverages, etc.) by patients who note a correlation with GERD symptoms is reasonable.
FROM Dr. Reina Bender, a gastroenterologist at the West Chester Gastrointestinal Group, and shared at PA Eats