Autoimmune Inner Ear Disease (AIED)
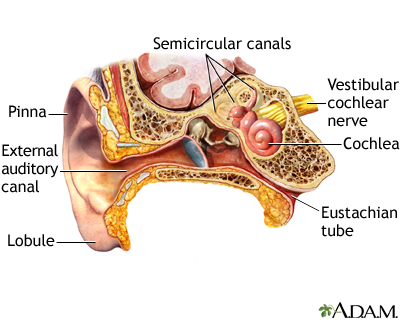
Autoimmune disease of the inner ear is part of the large group of neurosensory hearing losses, of which it represents less than 1%. The disease is defined as a rapidly progressive, often fluctuating bilateral sensorineural hearing loss, which evolves over a period of weeks or months and which initially responds to immunosuppressive therapy.
The diagnosis of AIED is still problematic as there are no reliable specific tests: it is mainly based on clinical evaluation and experience and must be suspected whenever we are evaluating a patient with a rapidly progressive idiopathic sensorineural hearing loss.
Menière’s Disease
Menière’s disease (MD) is a clinical disorder defined as the idiopathic syndrome of endolymphatic hydrops and characterized by a triad of fluctuating vertigo, tinnitus, and sensorineural hearing loss (with aural fullness).
Bilateral Vestibulopathy (BVP)
This disease was called in 1989 by Baloh as “idiopathic bilateral vestibulopathy” [39] and was recently defined in a consensus document by the Classification Committee of the Bárány Society [40]. The prevalence of BVP in adults is estimated to be 28/100,000 [41], and the mean age of onset is around 50–60 years; often, there is a diagnostic delay due to unclear symptoms and signs.
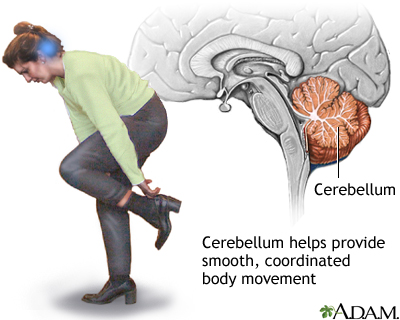
The BVP develops in most cases slowly and progressively; in the initial phase of the disease, patients can report recurrent short-term episodes of vertigo, with or without association of hearing loss. Both labyrinths and/or vestibular nerves can be affected, simultaneously or sequentially. The symptoms in BVP are caused by the sensory vestibular impairment leading to insufficent vestibulospinal reflexes. This disease has a negative impact on social and physical functions, with decay of the health-related quality of life in 90% of the patients.
The diagnosis is based on patient anamnesis (movement-dependent postural imbalance and unsteadiness of gait) and clinical finding (bilaterally reduced or absent function of the VOR). Symptoms are exacerbated in darkness and on uneven ground, because they depend more on visual and somatosensory control, and they can disappear under static conditions; some patients can present movement-induced oscillopsia, for example, during rapid head turns.
Diagnostic criteria for bilateral vestibulopathy (BVP) have been defined by the Classification Committee of the Bárány Society:(a)Chronic vestibular syndrome with the following symptoms:
unsteadiness when walking or standing plus at least one of 2 or 3;
movement-induced blurred vision or oscillopsia during walking
or quick head/body movements; and worsening of unsteadiness
in darkness and/or on uneven ground(b)No symptoms while sitting or lying down under static conditions(c)Bilaterally reduced or absent angular VOR function documented by
bilaterally pathological horizontal angular VOR gain <0.6, measured
by the video-HIT or scleral-coil technique, and/or reduced caloric response,
and/or reduced horizontal angular VOR gain <0.1 upon sinusoidal stimulation
on a rotatory chair and a phase lead >68 degrees(d)Not better accounted for by another disease
SOURCE