Skin problems that occur with Sjogren's syndrome include:
- dry, rough skin, called xerosis.
- small "blood spots" on the lower legs due to vasculitis, or inflammation of the blood vessels, called purpura.
- skin lesions that may appear as lumps, blisters, or ulcers, called vasculitis.
- red, ring-shaped lesions with a pale area in the middle, called annular erythema.
Skin concerns in Sjogren's Syndrome (Read this text or watch the video below)
About half of the people who have Sjögren's have dry skin.
Some experience only itching, and it can be severe.
Others develop cracked, split skin that can easily become infected. Infection is a risk for people with itchy skin, too, particularly if they scratch vigorously. The skin may darken in infected areas, but it returns to normal when the infection clears up and the scratching stops.
To treat dry skin, apply heavy moisturizing creams and ointments three or four times a day to trap moisture in the skin.
Lotions, which are lighter than creams and ointments, aren't recommended because they evaporate quickly and can contribute to dry skin.
Also, doctors suggest that you take only a short shower (less than 5 minutes), use a moisturizing soap, pat your skin almost dry, and then cover it with a cream or ointment.
If you take baths, it's a good idea to soak for 10 to 15 minutes to give your skin time to absorb moisture.
Having a humidifier in the bedroom can help hydrate your skin, too.
If these steps don't help the itching, your doctor might recommend that you use a skin cream or ointment containing steroids.
Some patients who have Sjögren's, particularly those who have lupus, are sensitive to sunlight and can get painful burns from even a little sun exposure, such as through a window.
So, if you're sensitive to sunlight, you need to wear sunscreen (at least SPF 15) whenever you go outdoors and try to avoid being in the sun for long periods of time.
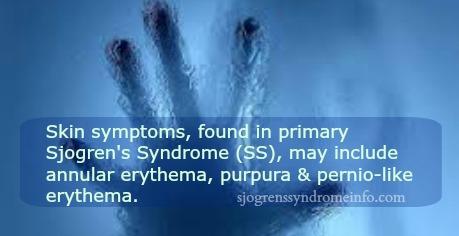
Rash is not a common finding in SS, and is reported in 10– 30% of patients. The rash is most commonly a nonpalpable purpura in the lower extremities, but can have other presentations as well.
Spending time in the sun may cause a skin rash.
The most important pathological findings in the skin biopsies of pSS include benign hypergammaglobulinemic purpura of Waldenstrom, leukocytoclastic vasculitis, and urticarial vasculitis (Sjögren's syndrome in dermatology. Fox RI, Liu AY)
Hypergammaglobulinemic purpura of Waldenström is characterized by hypergammaglobulinemia, recurring purpura, an elevated erythrocyte sedimentation rate, and the presence of rheumatoid factor indicative of circulating immune complexes. There is a significant association with autoimmune diseases, especially Sjögren's syndrome and lupus erythematosus.
Hypergammaglobulinemic purpura associated with Sjögren's syndrome and chronic C type hepatitis.
Skin Findings in a Patient with Sjogren’s Syndrome
Cutaneous purpura of Sjögren syndrome successfully treated with hydroxychloroquine. In Sjögren patients with various skin manifestations who are unresponsive or unable to tolerate high-dose steroids, hydroxychloroquine may be an effective option.
Hypergammaglobulinemic purpura in systemic autoimmune rheumatic diseases: predictive value of anti-Ro(SSA) and anti-La(SSB) antibodies and treatment with indomethacin and hydroxychloroquine.
In a study that examined the classification and clinical presentation of vasculitis in SS patients, 9 of 70 patients with primary SS developed vasculitis of small- or medium-sized vessels.
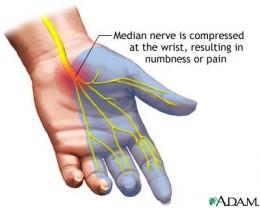
Leukocytoclastic vasculitis (LCV) is a term that describes the microscopic changes seen in various types of vasculitis affecting the skin and internal organs.
Vasculitis (inflammation of blood vessels) from DermNetNZ. This develops in about 10% of patients with primary SS and affects the skin in half of them (cutaneous small vessel vasculitis). Skin lesions usually present as multiple purple or reddish brown spots. The colour is due to bleeding from small inflamed vessels. Vasculitic skin lesions are most common and prominent on the legs but can develop anywhere. They may present as red flat patches, raised lumps, blisters, ulcers or a raised urticaria-like weals.
If vasculitis occurs, the doctor may prescribe drugs to suppress the immune system, such as cyclophosphamide.
Other skin changes that have been reported in Primary SS include:
- Annular erythema (ring-shaped red patches) has been noted in Japanese patients
- Livedo reticularis
- Erythema nodosum
- Diffuse hair loss
- Vitiligo
- Raynaud phenomenon
Vasculitis in Sjögren’s Syndrome patients also have disease in other organs. One of the most common extraglandular manifestations is vasculitis. Skin vasculitis, with palpable purpura clinically and leukocytoclastic vasculitis on pathological examination, is common. Although half of those individuals with subcutaneous vasculitis have only a single episode, skin vasculitic involvement is associated with more severe disease.
Vasculitis in Sjogren’s Syndrome
Urticarial Vasculitis is a form of vasculitis affecting the skin characterised by inflammation of the small blood vessels.